Why are scientific publications important?
Scientific publications, commonly referred to as papers, are how scientists share their own work or review the work done by others. In order to be accepted for publication in a journal, they must first be approved by experts in the field (“peer-reviewed”). As such, they are a testament to a scientific team’s credibility and the quality and reliability of their work. Both the stamp of approval given by a publication, and the ability of other scientists to learn about and build upon a team’s research, are important steps to take lab science closer to real-life benefits for humans. This publication is an original research article, in which a team of scientists share their own work and discoveries.
Where was this paper published and who are the team behind it?
This paper, under the full title “Combination of Interleukin-15 With a STING Agonist, ADU-S100 Analog: A Potential Immunotherapy for Prostate Cancer”, was published in the journal Frontiers in Oncology. The publication is open access, meaning the information is available to readers at no cost, and the journal’s Impact Factor (a measure of a journal’s influence in academic research circles) is 4.848.
The researchers who contributed to this paper are , Efthymia Papaevangelou, Prokar Dasgupta and Christine Galustian. They are based at King’s College, London, where this work was carried out. Prokar Dasgupta also works at the Urology Centre in Guy’s Hospital, London.
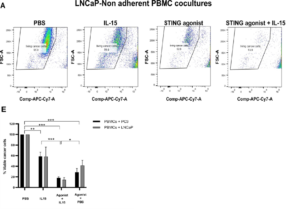 Figure 1 shows the number of cells that are left alive after 48 hours with IL-15, or IL-15 combined with the STING agonist. (A) Displays the increased killing of prostate cancer cells with STING agonist and IL-15 compared with IL-15 alone, STING agonist alone, or a control (PBS). (E) Displays the percent of living cancer cells after treatment.
Figure 1 shows the number of cells that are left alive after 48 hours with IL-15, or IL-15 combined with the STING agonist. (A) Displays the increased killing of prostate cancer cells with STING agonist and IL-15 compared with IL-15 alone, STING agonist alone, or a control (PBS). (E) Displays the percent of living cancer cells after treatment.