Slowing Cancer and Increasing Survival
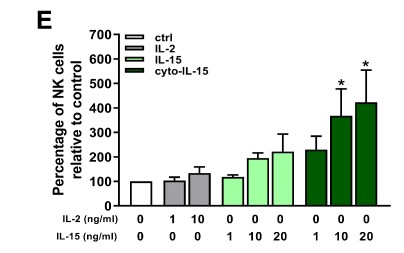
The researchers engineered IL-15 and two other drugs, antibodies called anti-CTLA-4 and anti-PD-L1, so that they could attach to cells. The results of this study proved, firstly, that the engineered drugs worked: they could attach to cells, and lab-based tests, in cells, showed that they could increase the population of a type of immune cell called Natural Killer (NK) cells, which play important roles in fighting both viruses and tumour cells. The engineered IL-15 also resulted in dramatic genetic changes in cancers in mice, affecting many genes normally involved in how cells move, and how they reproduce.
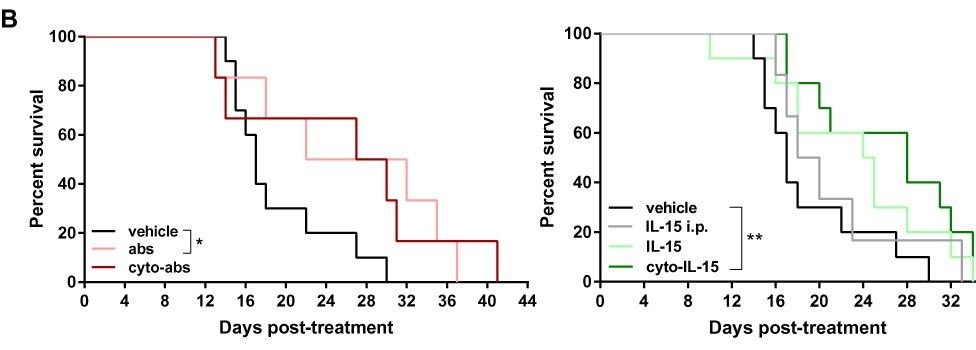
But the most exciting findings were that the engineered IL-15, both when it was used on its own and when it was used with the other two antibodies, not only slowed down the growth of tumours in mice by 52% (just engineered IL-15) and 58% (both engineered IL-15 and antibodies), mice treated with them also lived longer. The statistical analysis carried out on these results showed that they were most likely not due to chance, but were due to the treatments working. And, these mice didn’t appear to suffer any side effects.