Hormone Therapy: Old Dog, New Tricks
Project Summary
About the Researchers
Professor Iain J McEwan
Principal Investigator
Iain has been based at the University of Aberdeen since 1997. In 2009, he was promoted to a personal chair in Molecular and Cellular Endocrinology. Iain’s group focuses on investigating the molecular mechanisms of the androgen receptor and translating discoveries to the clinic.
Dr Irene Hunter
Co-Investigator
Irene has extensive research expertise in cell biology having worked at the Biocentrum (Basel) and the Karolinska Institute (Stockholm). For the last seven years, she has been investigating androgen receptor signalling in prostate cancer cells.
Dr Craig Jamieson
Co-Investigator
Craig has extensive experience in medicinal chemistry having worked in both industry (Merck Research Laboratories, GlaxoSmithKline R&D) and academia. His main research interests include structure based design and chemical synthesis of small molecules.
We are delighted to announce that this project has been awarded The Gordon Nicol Award, in honour of Gordon Nicol’s contribution to prostate cancer research.
Hormone Therapy
Hormones are chemicals that are used to send messages to different parts of the body. Male hormones like testosterone drive the growth and spread of prostate cancers by attaching to a protein called the androgen receptor. This ‘switches on’ the androgen receptor and it sends messages to the cancer cell to tell it to grow and divide. The androgen receptor is made up of three different parts: the part that male hormones attach to, the part that tethers the receptor to DNA and the part that sends the message to switch on or off genes in the cancer cell.
Hormone therapy disrupts this process either by reducing the production of male hormones or by preventing male hormones from attaching to the androgen receptor and switching it on. Hormone therapy sticks to the part of the androgen receptor that usually attaches to male hormones, meaning there is no room for the male hormones to attach.

The androgen receptor (AR) is a protein which is switched on by hormones called androgens. When it is switched on, it sends messages to the prostate cancer cells telling them to grow and divide.
The Problem with Hormone Therapy
Unfortunately, for many prostate cancer patients, hormone therapy will eventually stop working.
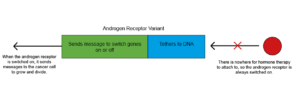
Prostate cancers can develop resistance and will continue to grow and spread despite ongoing treatment. One reason for this is the androgen receptor itself changes, so that the part that normally attaches to the hormone is missing. There’s nowhere for the hormone therapy to stick to, and so the receptor is always switched on. Therefore, messages telling the cancer cell to grow, and divide continue to be sent. These forms of the androgen receptor are known as androgen receptor variants (ARVs).
There are currently no treatments that can overcome this resistance which makes it an important target for research.
Prostate Cancer Research funded researcher Professor Iain J. McEwan talks about his work exploring new approaches to hormone therapy to keep it working for longer
Iain and his team are researching new drug combinations which target the androgen receptor in a different way to hormone therapy.
This could lead to new treatments for advanced forms of prostate cancer that continue to work beyond resistance to current drugs. These treatments would improve outcomes for prostate cancer patients and could also reduce side effects.
The Research Project
The researchers will target drugs to a different, but equally important, part of the androgen receptor: the part that sends the signal to switch on or off genes inside the cancer cell. Targeting this part of the androgen receptor means that treatments will still work on androgen receptors that are missing the part that usually attaches to male hormones.
They will use two different types of experimental drugs to do this: small drugs, and new protein drugs called SoloMERs. The small drugs will be used to stop the androgen receptor sending the messages telling the cell to grow and the SoloMERs will lock the androgen receptor into place so that the small drugs have a better chance of working. The team hope that this strategy can be used to ‘switch off’ both normal and drug-resistant androgen receptors.

““We aim to develop novel ways of switching off the activity of a protein called the androgen receptor, which is key to prostate cancer cell survival. Our highly innovative, and collaborative, approach marries medicinal chemistry (Dr Craig Jamison, University of Strathclyde) with biologics (protein-based drugs), developed in partnership with Elasmogen Ltd, a biopharmaceutical company. If successful this has the potential to significantly improve the outcome for men with advanced disease.”
Professor Iain McEwan
University of Aberdeen