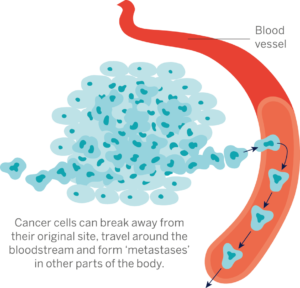
Dr Magali Williamson and Dr Ritu Garg lead our ‘Stopping the spread’ project which focuses on preventing the spreading of the cancer cells by investigating the cellular changes which underpin metastasis. The team recently completed the second year of their five-year PCR project and you can read about this year’s exciting findings below.