Mapping differences in treatment patterns
Project Summary
About the Researchers
Dr Robert Horne
Principal Investigator
Rob Horne is Professor of Behavioural Medicine at UCL School of Pharmacy. His research focuses on the role of psychological and behavioural factors in explaining variation in response to treatment.
Rob trained in pharmacy and health psychology. A key theme in his research is the understanding of patient and public perspectives of illness and treatment and how this can be applied to help get the best from essential treatments for the benefit of individuals and society. His work has resulted in internationally applied tools and guidelines for supporting adherence to treatment and improving patient care.
Dr Jonathan Shamash
Principal Investigator
Dr Zoe Moon
Co-Investigator
Dr Zoe Moon is a Senior Research Fellow at the Centre for Behavioural Medicine in the School of Pharmacy at UCL, and a Senior Behavioural Science Consultant at UCL Business Company Spoonful of Sugar. Prior to joining UCL in 2021, Zoe worked at the Health Psychology Section at King’s College London where she completed her PhD in 2017 and worked as a Postdoctoral Research Associate and Teaching Fellow.
Zoe’s research focuses on applying behavioural medicine and health psychology to supporting patients with long term conditions, most specifically around medication adherence. This includes conducting insights research and designing and evaluating behaviour change and self-management interventions. Zoe has a special interest in psycho-oncology, particularly around prostate and breast cancer. Her research interests also include digital health and health inequalities.
Dr Kenrick Ng
Co-Investigator
Kenrick Ng is a final year specialist trainee in Medical Oncology at University College London Hospitals and Barts Health NHS Trust in London,UK. He obtained his medical degree from the University of Cambridge in 2012, and continued his postgraduate training in major cancer centres in London prior to obtaining his Speciality Certificate in Medical Oncology in 2020. He completed a PhD in Cancer Immunology in 2021 with the UCL Cancer Institute, while concurrently working in early phase clinical trials in the NIHR UCLH Clinical Research Facility.
Kenrick has a special interest in the treatment of genitourinary cancers, particularly prostate and testicular cancers. In particular, his research focuses on factors which may impact on healthcare engagement and survivorship issues for patients on or who have received anti-cancer treatment. His research work in the field has been awarded with the Helen Patterson Research Registrar Award at the British Uro-Oncology Group Meeting of 2019, and the ASCO GU Merit Award in 2020. While he is a full-time clinician, he has published extensively and has more than 50 peer-reviewed papers and book chapters. He is also on the editorial board of the journal Oncology and Therapy, and is a special issue editor on Global Disparities in Genitourinary Cancers with Frontiers in Urology.
Dr Edward Christopher Dee
Collaborator
Edward Christopher "Chris" Dee is a resident in the Department of Radiation Oncology at Memorial Sloan Kettering Cancer Center in New York City. Prior to residency training, he completed his medical studies at Harvard Medical School where he also conducted prostate cancer clinical research at the Dana-Farber Cancer Institute. He holds a bachelor's degree in molecular biophysics and biochemistry from Yale University.
Chris's research interests focus on health services for people with cancer as well as access to prevention and screening for people at risk of cancer. He has a deep interest in local and global disparities and has done work highlighting the need for equity particularly for minoritized groups in the US. He also conducts research in the Philippines and Southeast Asia, where he is from; his work in the region focuses on issues of cancer care access in lower-resource settings. He has published extensively in The Lancet, The Lancet Oncology, JAMA Oncology, Cancer, JCO Oncology Practice, JCO Global Oncology, and others.
With the PCR collaboration, Chris hopes to further our understanding of the mechanisms that underlie inequities in care, such that interventions may be better designed to improve access for those who need it the most.
The problem with clinical trials
Clinical trials are an important step in developing and testing new treatments.
How well medicines work and how safe they are can change depending on a person’s age, gender, ethnicity and more, so it is vital that clinical trials include a diverse range of participants. Black men are twice as likely to be diagnosed with prostate cancer compared to White men, and 2.5 times more likely to die from the disease. However, despite Black men being more likely to get it, they are under-represented in prostate cancer trials.
As a result, clinical trials do not account for the differences in benefits and/or side effects of treatments in Black men. This means that we don’t know whether treatments will work as well or if they could cause worse side effects in Black men compared to White men. There is also concern that Black men are more likely to decline or not complete their prostate cancer treatment.
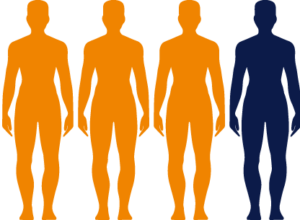
1 in 4 Black men will be diagnosed with
prostate cancer
Robert, Jonathan and the team will educate healthcare professionals and make sure that they know how to support Black men through treatment. Ultimately, this will mean that Black men diagnosed with prostate cancer will be better supported to stick to and get the best from treatment.
The research project
The research team, led by Robert and Jonathan, will look through NHS records to see if there are any patterns showing if men from different ethnicities are more or less likely to choose and stick to different treatments. They also hope to expand on previous research that showed Black people are more likely to benefit from hormone therapy.
They will also conduct in-depth interviews and questionnaires with Black men diagnosed with prostate cancer to uncover what stops men from continuing with their treatment and how they could be better supported. They will develop targeted support specifically designed to help Black men with their prostate cancer treatment.
The researchers also aim to gain a better understanding of the most appropriate treatments for Black patients. This would mean that we can select treatments for patients to ensure the best outcomes and fewer side effects.

Overall, this study will promote a greater understanding of the systemic barriers to care faced by Black men, including socioeconomic and cultural factors. The team hope to identify key points which lead to poorer engagement of ethnic minorities in healthcare and encourage better outcomes for them.