Hormone Therapy: Stopping resistance in its tracks
Project Summary
About the Researchers
Dr Luke Gaughan
Principal Investigator
Dr Luke Gaughan is a senior lecturer at Newcastle University. He has worked on several exciting projects studying the mechanisms of androgen receptor regulation in prostate cancer.
Dr Dominic Jones
Research Associate
Dominic is a research associate at Newcastle University. He will be using cutting edge technology to identify the key proteins involved in the production of androgen receptor variants and the growth and spread of prostate cancer.
We are delighted to announce that this project has been awarded The Martin Dallison Award, in honour of Martin Dallison’s contribution to prostate cancer research.
Hormone Therapy
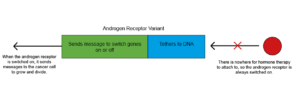
Hormones are chemicals that are used to send messages to different parts of the body. Male hormones like testosterone drive the growth and spread of prostate cancers by attaching to a protein called the androgen receptor. This ‘switches on’ the androgen receptor and it sends messages to the cancer cell to tell it to grow and divide. The androgen receptor has three different parts: the part that male hormones attach to, the part that tethers the receptor to DNA and the part that sends the message to switch on or off genes in the cancer cell.
Hormone therapy can stop male hormones switching on the androgen receptor. It sticks to the part of the androgen receptor that usually attaches to male hormones, meaning there is no room for the male hormones to attach.

The androgen receptor (AR) is switched on by hormones called androgens. When it is switched on, it sends messages to the prostate cancer cells telling them to grow and divide.
The Problem with Hormone Therapy
Unfortunately, for many prostate cancer patients, hormone therapy will eventually stop working.
One reason for this is the androgen receptor itself changes, so that the part that normally attaches to the hormone is missing. There’s nowhere for the hormone therapy to stick to, and so the receptor is always switched on. Therefore, messages telling the cancer cell to grow, and divide continue to be sent. These forms of the androgen receptor are known as androgen receptor variants or ARVs. ARVs are found in around 70-80% of advanced prostate cancer patients.
At the moment, we don’t know how ARVs are made. Therefore, we don’t know how we can stop this process and keep hormone therapy working for prostate cancer patients.
Prostate cancers develop resistance to hormone therapy when shortened versions of the receptor called ARVs are formed.
Prostate Cancer Research funded researcher Dr Luke Gaughan talks about his work investigating how prostate cancers become resistant to hormone therapy.
Luke and his team are investigating how ARVs are made and how this process could be stopped to prevent hormone therapy resistance.
This would lead to a new and better way to treat advanced prostate cancer that lasts longer than current therapies. Resistance to hormone therapy could be delayed, reversed, or even avoided completely.
Luke and Dominic's Research Project
The researchers have developed cutting-edge technology in order to give them powerful insights into how ARVs are made in advanced prostate cancer cells. They will identify key proteins that are involved in ARV production and the growth and spread of prostate cancer. The researchers will then conduct further tests to establish whether these proteins have the potential to be drug targets. Once potential targets have been established, drugs could be developed that block these proteins, stopping the production of ARVs and preventing resistance to hormone therapy.

““Together with my co-leads on the PCR-funded project Mr Rakesh Heer, Consultant Urological Surgeon, and Prof Craig Robson, we will be undertaking a super novel approach to study how we can prevent advanced prostate cancer-associated forms of the androgen receptor being generated. By blocking this process we will be able to prevent disease progression. We are thrilled to be part of the national PCR research team and are very much looking forward to helping deliver new targets for future treatments to help men with prostate cancer.”
Dr Luke Gaughan
Newcastle University