A blood test to revolutionise early detection
Project Summary
About the Researchers
University of Cambridge
Dr Harveer Dev
Principal Investigator
Harveer is a group leader and academic urologist at the University of Cambridge Early Cancer Institute. His research group are interested in what makes early prostate cancer lethal, and how best to intervene to improve survival. He is leading research efforts to explore the epigenetic landscape of prostate cancer, and how these insights can be applied using liquid biopsies in the clinic.
We need more reliable ways to diagnose PC
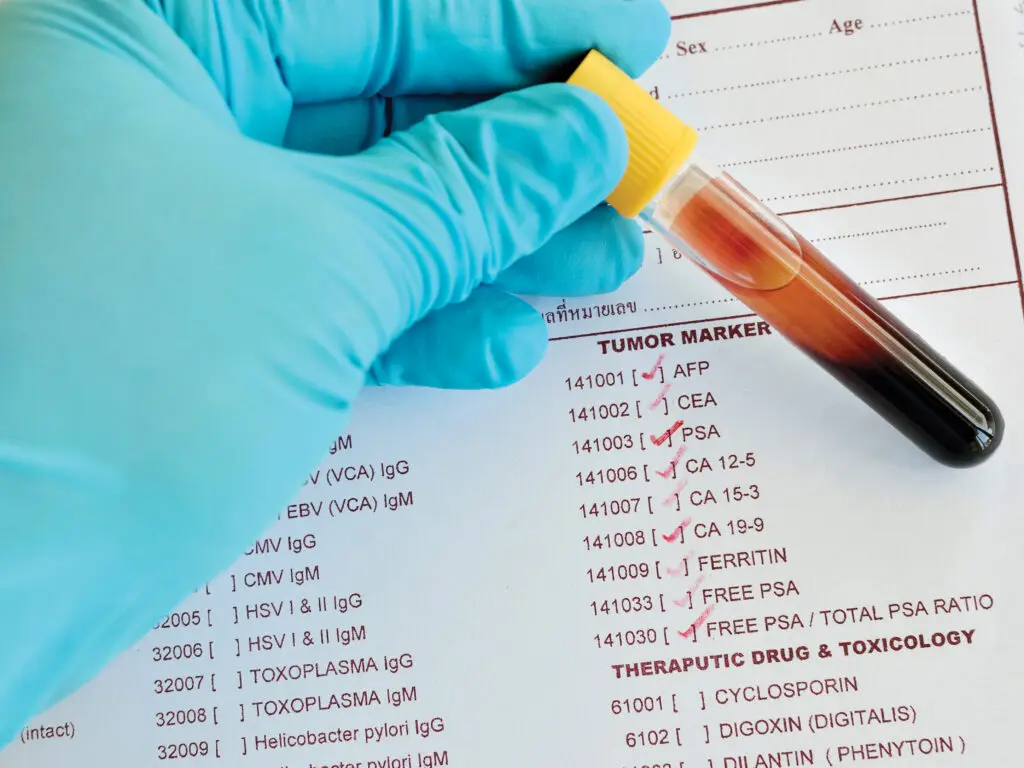
We know that catching cancer early saves lives. But prostate cancer is behind the curve in terms of the technology we have available. The PSA test is widely used but not as reliable as we need it to be. When the PSA test gets it wrong, it can lead to some aggressive cancers being missed. It can also lead to unnecessary biopsies and anxiety for men who have raised PSA but do not have cancer. While MRI scans can improve the accuracy of diagnosis, they are not available to everyone.
One in eight men in the UK are diagnosed with prostate cancer. But for many, the disease progresses very slowly, meaning these men may not need treatment. A more accurate way to diagnose prostate cancer could lead to more men who need treatment being treated more successfully and men who don’t need treatment being able to safely live without its side effects.

The Research Project
Changes in how some genes are switched on or off (the methylation levels) could potentially tell us the difference between low-risk and high-risk cancers. So far, though, it has been hard to detect these changes in the blood as there is such a tiny amount of material that a test can pick up. The research team has developed a test that could get over this hurdle by testing thousands of cancer signals at once. Because they used a larger ‘net’ to capture our targets of interest, this exciting new approach has a higher chance of picking up cancer-specific signals and performs better than PSA and other blood tests. Thanks to PCR funding, the researchers will validate their test in more than 1000 samples from the UK, Europe and Africa.
This will show how well the test performs across various settings and ethnicities: vital information if the test is to be approved. Because the study includes samples taken 20-30 years ago, we can see how well we can predict deadly cancer years in advance. This could help find which patients need more treatment earlier on.
What will this mean for patients?
This new blood test could transform the diagnosis of prostate cancer, give men with a prostate cancer diagnosis more clarity about what their diagnosis means and whether they should be treated or not, and will help to pave the way for a national screening programme.